3 Secrets to Getting Your Patients to Collaborate in the Treatment Plan
November 12, 2014
By Robert Striks, Special Writer, Encompass HealthCare & Wound Medicine
There's a funny scene in the Marx Brothers movie, "Horse Feathers," where Chico tells Harpo how to escape from the room they are locked inside by using a rope. Chico instructs Harpo to tie one end of the rope to the bed and then throw the other end of the rope out the window. "Tie on the bed, throw the rope out the window," he repeats. Haplessly, Harpo takes the tie he was wearing around his neck, places it on the bed and then throws the entire escape rope out the window.

What's the worst that could happen?
Not fully understanding the doctor's instructions is just one of the many reasons why patients don't comply with their treatment plans. Just consider the old expression, "that's a tough pill to swallow," which has its roots in medicine, and you get it. It's not always a piece of cake to follow a physician's advice and sometimes it's downright painful. Anyone who's ever gone through physical therapy knows that.
But before I get into the secrets to getting your patients to comply with your treatment plans, I want to say something about the word, "Compliance."
I don't like the word compliance.
It sounds like I have to give up something. Compliance sounds like compromise and while compromise may be the secret to a happy marriage, it's not a good match with medicine.
There's just not enough warm and fuzzies in the word compliance. So I'm proposing we change the term to patient "collaboration." Everyone wants to collaborate, right? Things get accomplished and with greater success when there's collaboration.

Success happens when doctors collaborate with their patients.
Collaboration Secret #1: Communicate the Benefits of the Treatment to the Patient
If we really want our patients to collaborate with us on their treatment plans, there's no better place to start than that easy, three to four credit course called Advertising 101. In that class, the first thing you learn is to define the benefit(s) of a product and then drive those benefits home to the consumer in every creative way possible.
For example, let's say you want your patient to check their blood glucose three times a day before meals. Diabetic patients are notorious for not "complying" with this request. The supreme benefit to the patient is dramatically improved control over their diabetes. This is an important distinction because sometimes we explain the benefits of a treatment and it comes off like we're the ones who will benefit. That would be a miscommunication, as it should always be about the patient benefitting.
DOCTOR: I'd like you to check your sugars three times a day and record your results.
Versus:
DOCTOR: You're going to be amazed at how well you can control your sugars when you test three times a day.
Listening from the patient's point of view, which delivery would make you more likely to collaborate with the doctor?
But everyone is unique in how they process information. So a one-style-fits-all approach to presenting the information won't work. One patient may respond favorably to a complete dissertation on the treatment, where another is more collaborative when the information comes in doses or intervals.
Here, it's helpful to see patient collaboration as something you bring to the doctor-patient relationship and not as something that is incumbent on the patient to perform. The onus is on you, the physician, to vary your delivery so that the individual patient is encouraged to cooperate.
Collaboration Secret #2: Identify and Eliminate Obstacles to Patient Collaboration
Again looking back to our undergrad studies, if you took Communications 101 in college, you know that the words you say are only a small fraction of the total engagement that happens when you're communicating with your patient. Nonverbal communication, how you say the words you say, can make up as much as 98%. The tone in your voice, a sigh, eye contact, touch and facial expressions are often more persuasive and more telling than the actual words spoken.
Knowing that, one has to ask, "What am I bringing to the conversation that is interfering with my patient wanting to collaborate with me?" In other words, what am I doing through my gestures, tone and context that gets in the way of my patient buying in to my treatment plan?
This isn't an easy concept to grasp since deep down, many of us think the mere fact that we endured all that medical training means that patients should do what we tell them to do. But that attitude provides precisely the kind of context that comes shining through our interactions with our patients and obstructs collaboration.
Collaboration Secret #3: Consider Your Context
Here's a quick anecdote about this topic. At one time, I was thinking about becoming a food distributor/salesman to restaurants. I asked a major supplier in the area if I could shadow their top salesman to see what the job was like. They agreed. As we pulled up to one of his customers, the salesman said, "Wait until you meet this guy. He gives me a hassle every time I call on him."
Sure enough, when we all sat down to talk about the week's order, the customer was combative and not very agreeable to the salesman. But when the salesman stepped away to check the customer's inventory, the customer opened up to me about his distrust of the salesman and his hesitance to give the salesman more of his business. I asked about the challenges of running his store and we talked for nearly a half hour before the salesman returned. The customer and I had brainstormed some good ideas and the salesman was quite amazed by how the customer responded to me.
Why was there such a disparity between the way I was treated and the way the salesman was treated by the customer? It's really quite simple. When I heard the salesman disparage the customer as we pulled up, I immediately filled my brain with one context for this customer. My context was "this customer needs me to use my talents and expertise to grow his business." As a result, that is exactly who showed up for me – a customer who was ready to collaborate. The salesman, on the other hand, had the context, "Shoot, I've got to meet with this hassling guy again" and that's who showed up for him.
The point is that we can adopt whatever context we choose depending on the individual patient. We can have a positive predisposition for the patient regardless of our history with him or her. We can determine who shows up for us in every doctor-patient interaction. But it's something we have to do. It's incumbent on us to adjust our mindsets because they're the only mindsets over which we have any real control.
Give it a try on your next set of patients. Take a few critical moments before knocking on the exam room door to establish a context for yourself. Ask yourself, "Who do I want to be with this patient so he or she will collaborate with me on treatment?" The answer might be, just for example, "I'm going to be the trustworthy kiosk of information for this patient because they're going to have a hundred questions about their diagnosis."
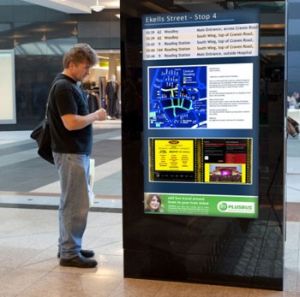
As a kiosk of information, you're not going to become overly emotional with this patient because kiosks don't emote. You're not going to talk over this patient's head because kiosks of information are usually designed to accommodate all levels of education. You can trust a kiosk of information to be there for the entire time needed for acquiring that information. So you're not going to be rushing the patient to get to your next patient. You're going to give that patient all the time they need to process the information.
Kiosks of information are friendly and non-judgmental. That's who you're going to be. Now, who do you think will show up for you in that context? It'll probably be someone ready to process information from a trusted source that is friendly and non-judgmental.
Now you can begin to see the benefits of creating a very specific context for each of your doctor-patient interactions – unburdened by any negative attitudes or preconceptions you may have for the patient.
If you stayed with me through that exercise, you have a lot to think about. I'll be back in the future to expand on patient collaboration with more techniques for encouraging your patients to become healthier.
About the Author
Robert Striks is a writer and marketer for Encompass HealthCare & Wound Medicine in West Bloomfield, Michigan. He is Dr. Bruce Ruben's medical editor and blogs frequently on healthcare-related topics. His email address is r.striks@encompasshealthcare.com.
Dr. Bruce Ruben is the Founder and Medical Director of Encompass HealthCare, located in West Bloomfield, Michigan. Encompass Healthcare is an outpatient facility featuring advanced wound care, IV antibiotic therapies, hyperbaric oxygen treatment, nutritional assessment, and other treatment modalities. Dr. Ruben is board certified in Internal Medicine, Infectious Disease, and in Undersea and Hyperbaric Medicine. He is a member of the Medical and Scientific Advisory Committee and National Spinal Cord Injury Association (NSCIA) board.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.







