Antimicrobial Stewardship in Action
March 31, 2021
Antibiotic resistance is a growing health threat, not just in the United States, but throughout the world. Health care professionals are facing problems with antibiotic resistance, as well as with resistance to other antimicrobial agents. The Centers for Disease Control and Prevention (CDC) noted in 2019 that “more than 2.8 million antibiotic-resistant infections occur in the United States (US) each year, and more than 35,000 people die as a result.”1
The CDC lists 18 current threats, with three on the watch list as emerging causes of antibiotic resistance. Many of the bacteria on this threat list are found in chronically stalled wounds. Therefore, wound clinicians must be good stewards of antimicrobial treatments to prevent contributing to an already worsening problem.
Dressing Selection
Antimicrobial stewardship begins with appropriate dressing selection. Many dressings in the marketplace today include some form of an antimicrobial, such as silver, dialkylcarbamoyl chloride (DACC), iodine, medical-grade honey, and others. When used correctly and applied as indicated, antimicrobial dressings can be alternatives to antibiotic use. Clinical guidelines recommend that antimicrobial dressings be considered, albeit for short periods, for wounds where infection is confirmed or suspected or where bioburden may be excessive enough to delay wound healing. Continuation of an antimicrobial dressing is appropriate for longer once a wound is reassessed, and continued parameters and clinical judgment warrant ongoing application.2


Dressings that utilize DACC are potential alternatives to silver dressings. DACC irreversibly binds bacteria so that when the dressing is removed from the wound, it also removes the bacteria, thereby lessening the amount of bioburden with each dressing change. Because DACC-based dressings do not kill bacteria, there is no chance of cytotoxicity or cell debris remaining in the wound bed and further delaying healing.3 Some studies show that silver-resistant bacteria may be on the rise, however, so alternatives to silver dressings should also be considered.4
How much do you know about antimicrobial stewardship? Take our 10-question quiz to find out! Click here.
Topical Wound Cleansers
Another armament in the wound arsenal for many wound care professionals is the use of topical wound cleansers to reduce bioburden and bacterial count. This can range from products that use PSI to blast non-viable tissue and bioburden from the wound bed to cleansers that have a biocidal or virucidal mechanism of action. Hypochlorous acid and polyhexamethylene biguanide (PHMB) can be selectively biocidal or virucidal without harming mammalian cells.5 Various wound cleansing agents offer benefit by reducing antibiotic use and should be explored to determine the best fit for the wound and the patient. Some agents may alter the pH of the wound bed; some may utilize surfactants to assist with disruption of biofilm activity. It is important to verify that the cleansing agent does not interfere with other products when they are used synergistically, such as collagenase and surfactant cleansers, which can result in collagenase inhibition, for example.6
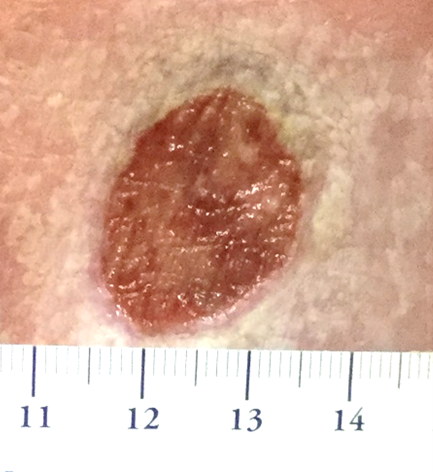

The first photo shows a wound with unhealthy tissue starting to form in the wound bed. The periwound shows maceration and leaves much to be desired. After 1 week of treating with a wound cleanser designed to reduce bioburden and bacteria count, we can see the wound bed appears healthier and the periwound is now normal. The wound is set to progress toward healing. Images provided courtesy of Wound Care Plus, LLC.
Other Treatment Modalities
Other modalities can also be utilized as part of an antimicrobial stewardship program. Sharp debridement is still the fastest form of debridement, quickly removing necrotic or non-viable tissue, which can be a source of bacterial growth and sepsis. This modality stimulates the wound bed to encourage new cell recruitment and possible tissue growth. Additionally, by removing non-viable tissue, we can gain access to underlying tissue where tissue cultures can be performed for evaluation of bacteria in the tissue. Tissue cultures allow for more accurate use of antibiotics targeted to tissue infection versus topical bacteria that could be wiped from the wound bed.


Polymerase chain reactions (PCR) testing in studies was shown to be more reliable and to identify hundreds more unique genera versus a significantly smaller number found with traditional cultures in one study. Sequencing and PCR testing, based on studies, show a high level of accuracy versus traditional cultures. Identifying bacteria accurately before treating with antibiotics is a form of antibiotic stewardship and should be considered.7
Conclusion
Antimicrobial stewardship is important for professionals involved in wound care. In today’s wound care practice, there are many options to assist with antimicrobial stewardship while encouraging wound healing. By incorporating one or more of these strategies and modalities, wound healing can be accomplished, and stewardship can be promoted.

References
1. Centers for Disease Control and Prevention. Antibiotic / antimicrobial resistance (AR / AMR). 2021. cdc.gov: https://www.cdc.gov/drugresistance/biggest-threats.html#:~:text=2019%20…. Accessed March 24, 2021.
2. Vowden P, Vowden K, Carville K. Antimicrobial dressings made easy. Wounds Int. 2011;2(1):1-6. https://www.woundsinternational.com/download/resource/6086. Accessed March 17, 2021.
3. Hajská M, Dragúňová J, Koller J. Cytotoxicity testing of burn wound dressings: first results. Cell Tissue Bank. 2017;18(2):143-151.
4. Finely PJ, Norton R, Austin C, et al. Evidence of emergent silver-resistance in clinical bacteria: a major implication for wound care and the use of silver-dressings. Poster presented at the Symposium on Advanced Wound Care, Spring 2015.
5. Chindera K, Mahato M, Kumar Sharma A, et al. The antimicrobial polymer PHMB enters cells and selectively condenses bacterial chromosomes. Sci Rep. 2016;6:23121. https://doi.org/10.1038/srep23121
6. Smith and Nephew. Santyl ointment compatibility. 2021. https://santyl.com/hcp/compatibility. Accessed March 24, 2021.
7. Giuliano C, Patel CR, Kale-Pradhan PB. A guide to bacterial culture identification and results interpretation. PT. 2019;44(4): 192-200.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











