The Challenge of Lower Extremity Wounds – Arterial Wounds, Part 2
June 8, 2017
Part 2 of a series discussing the assessment and management of lower extremity wounds For Part 1, click here.
As we move forward in our continuation of lower extremity wounds, we will now turn our attention to arterial wounds. In my previous post, we discussed challenges with venous leg ulcers. Lower extremity wounds continue to challenge clinicians on a daily basis. We often refer to them as "the big three" – or how I like to refer to them, "the pesky triplets." It doesn't matter what we call them, we know we are referring to venous leg ulcers, arterial ulcers, and diabetic foot ulcers. In no way shape or manner will we disregard the many other types of lower extremity wounds we may encounter as wound clinicians, but these three are the most common and often present with treatment challenges.
As we went over venous leg ulcers, we discussed that these wounds are associated with some type of venous insufficiency (among other possible complications) and of course, a lot of inflammation. As we move forward and dissect arterial wounds and etiology, we will also discuss assessment, location, characteristics, and treatment.
System Overview and Pathophysiology of Arterial Wounds
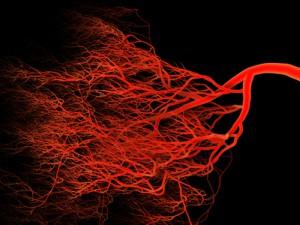
What is peripheral arterial disease (PAD)? PAD occurs when the arteries in the legs become narrowed or blocked by plaque build up, reducing blood flow to the affected extremity and leading to ischemia—and potentially necrosis.
PAD affects at least 12 million people in the United States alone, and is noted to be more common among people over the age of 50, especially those with history of smoking, hypertension, and/or heart disease (among other comorbidities such as anemia, arthritis, CVA, traumatic injury to limb, and hyperlipidemia). With the narrowing or blockage of vessels, a disruption in vascular supply occurs. The reduced flow will attribute to decreased perfusion/oxygenation and reduced nutrients, contributing to subsequent death of unnourished cells, ultimately causing skin changes.
It is very important to recognize and (with assistance of the skin, wound, assessment team, or "SWAT team") be able to diagnose this type of wound properly. Arterial disease is progressive, and rarely a stable condition. It is of utmost importance to treat in the early stages to prevent full progression of disease, have increased chances of positive outcomes, and decrease incidence of consequences as the disease process fully progresses.
Assessment of Arterial Wounds
Ankle-brachial index (ABI) testing is a very common, noninvasive test for the assessment of lower extremity perfusion. An ABI less than 0.8 indicates presence of arterial compromise. An ABI less than 0.5 will indicate severe arterial compromise. This requires the clinician to coordinate with SWAT to address findings, as well perform other exams and diagnostics to solidify findings. Other signs to look for in the assessment of arterial wounds include:
- Presence of hair loss on foot and leg
- Thin, smooth, shiny, taut, dry skin
- Atrophy of subcutaneous tissue
- History of claudication
- Dependent rubor and pallor on elevation
- Thick, yellow, brittle, ridged, and deformed toenails, hypertrophic nails
- Skin temperature changes to affected limb, cool to touch
- Absent/diminished pulses
- Pain may be present at rest
- Pain is severe and increases with elevation
- Paresthesia (numbness)
- Delayed capillary and venous filling time
- Decreased temperature
- Decreased healing time
Characteristics of Arterial Ulcers
As mentioned in my last post, this remains very appropriate for lower extremity wounds: LOCATION, LOCATION, LOCATION! Pinpointing the location of lower extremity wounds is important. Once we put all assessment parts and characteristics together, it's much easier to identify causes—and then of course—treat. Typically, arterial wounds have a tendency to occur distal, on the foot, at the tips of (or between) toes, over phalangeal heads, at pressure points from foot wear, and around lateral malleolus.
Other characteristics of arterial ulcers include:
- Punched out appearance
- Even wound margins
- Round
- Shallow to deep in depth
- Minimal drainage/exudate
- Wound bed pale, granular tissue rarely present
- Slough, eschar, necrosis, and gangrene may develop
- Periwound tissue, pale and non-stained, decrease in temperature, blanched or purpuric
- Infection is common yet masked, secondary to decreased perfusion/oxygenation, signs subtle
Diagnostics
There are several diagnostics that can be performed by a trained health care provider/practitioner that can assist with assessment of arterial ulcers. They include:
- Capillary refill time, normal less than 3 seconds
- Venous filling time is normally 10 seconds; greater than 20-30 seconds indicates severe ischemia
- Rubor of dependency: elevate and hold extremity for 60 seconds, place back to surface and check time it takes for color to reappear.
- Pulses 0/+1/+2/+3
- ABI (ankle-brachial index) > 1.2 calcified non compressible vessels, 0.9-1.1 normal, 0.5-0.8 mixed etiology, < 0.5 suggests severe PAD
- TBI (toe-brachial index) > 0.75 normal and < 0.5 abnormal
- Doppler studies
- MRA: magnetic resonance angiogram
- Segmental pressures
- TcpO2: transcutaneous oxygen
- Angiography (Gold Standard)
There is research done constantly, and I realize that this list of diagnostics is not inclusive of all methods available. Again, I am trying to educate, teach, coach, and mentor—please leave me a comment if you would like me to discuss other diagnostics not addressed in this post.
Arterial Ulcer Treatment Goals
Identifying arterial ulcers is complicated enough without having to discuss treatment. Factors such as stage of disease and extent of damage caused by narrowing or blockage of vessels will determine the treatment course. Unlike venous leg ulcers, where compression is often the "Gold Standard," arterial wound treatment is a bit more complicated. Proper perfusion and oxygenation are required, and the healing of wounds, localized wound care, and medication are not enough (the majority of the time) to fix the underlying factor: circulation.
Again, the use of the SWAT team remains as important as ever. Sound the horns, ring the bells, send the smoke signals, send Morse code, release the pigeons, and let's gather the troops because, you guessed it, "it takes a village!"
- Improve circulation, revascularization, vascular consult (bypass graft, angioplasty, stent application, arthrectomy, etc.)
- Medications - opinion differs among practitioners (pentoxifylline, antiplatelet agents, vasodilators such as cilostazol)
- Pain management and systemic antibiotics as needed
- Smoking cessation and other lifestyle changes
- Moist wound healing
- TIME, wound bed preparation, extra precaution with debridement due to compromised circulation
- Good nutrition and hydration
- Protect from further tissue damage, trauma
- Treat underlying infection when present, and prevent infection
- Hyperbaric treatment as appropriate
- Bioengineered skin equivalents
- Light compression may be indicated with patients that have mixed etiology and not severe PAD
Ending Points
As previously mentioned (and I will continue until I turn blue), coordination with the SWAT team is instrumental and of best practice. Local wound care using moist wound healing and wound bed preparation is essential, but be very careful with the debridement aspect of wound bed preparation. With arterial ulcers, involving the cardiologist and vascular surgeon early is a crucial part of the treatment—and a big piece of the SWAT team. Further educating ourselves, teaching our patients and their family members, and increasing awareness is a huge responsibility. We clinicians have a continued responsibility to teach, coach, and mentor. The demand is overwhelming, but a responsibility we are willing to take. Continue to refer to and follow guidelines.
Keep healing my friends!
Author's note: in part 1 of my post about venous leg ulcers, several different terms where used throughout. The majority of the current research identifies them as venous leg ulcers, although there is continued documentation in current literature that refers to those type of wounds as venous ulcerations, venous insufficiency ulcers, and venous stasis ulcers. Needless to say, the key word is "venous." My apologies if any confusion was caused as a result of my previous blog, and as always, I welcome constructive criticism. I love the energy and the involvement of readers.
About the Author
Martin Vera is a certified wound specialist with over 19 years of nursing experience, with a passion for wound management and patient-centered care.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.