Classifying Skin Care Moisturizing Agents: What Does My Patient Need?
September 8, 2016
There are currently hundreds of skin moisturizing products on the market for clinicians to choose from. It is often difficult to wade through various brands and formulations to determine which is appropriate to treat a specific skin issue, and even more is involved in understanding the function of each ingredient. Protecting the body’s functional barrier is integral to staving off pathogens and defending the body from infection. Have you ever encountered a dermatological issue in your daily practice and thought…what skin care product will best address this affliction? What does this patient’s skin need? Do we need to hydrate dessicated skin, lubricate to decrease friction, protect a broken barrier? In this installment, we will review the mechanism and function of three main types of skin moisturizing agents and how they can be best utilized in clinical practice for patients at risk for or experiencing altered skin integrity.
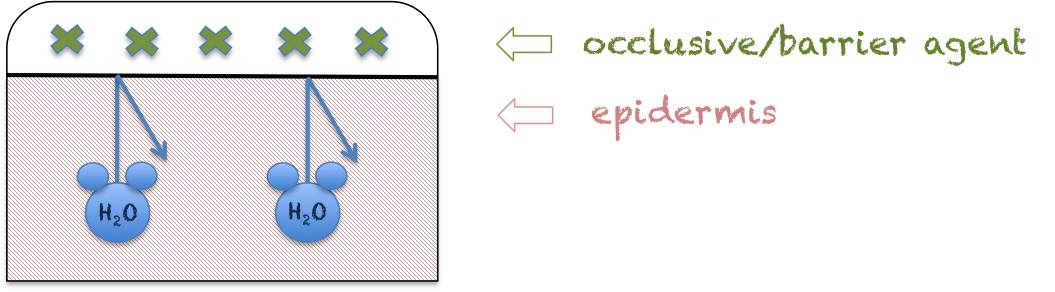
Barriers/Occlusives
Skin barriers work through providing a physical barrier over the epidermis to prevent trans-epidermal water loss (TEWL). These agents are generally oils (petrolatum, plant oils such as olive or coconut oil), waxes, and silicone formulations. Skin barrier products tend to be a little messy, don’t work well with clothing and become more viscous as temperature increases (and are therefore better for winter or severe dryness). They can sometimes cause irritation or folliculitis. Barrier products are often useful in protecting against development of incontinence-associated dermatitis (IAD).
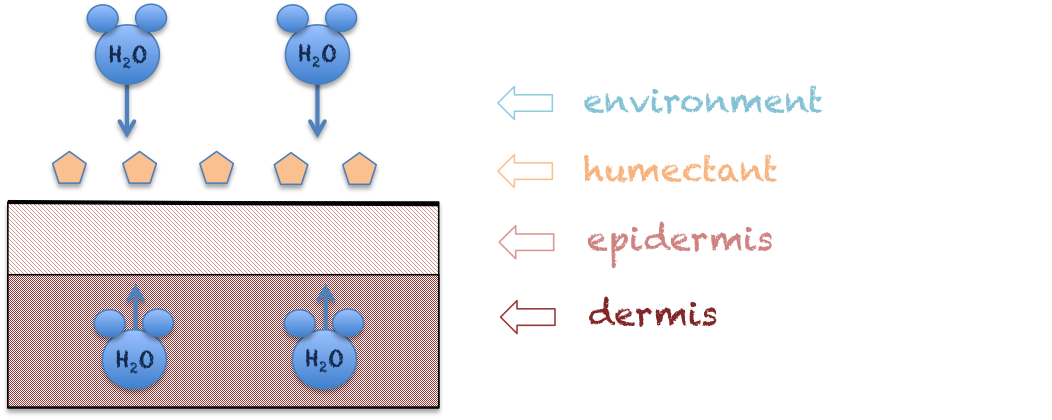
Humectants
Humectants are water-binding substances such as amino acids, sugars, and proteins that utilize an osmotic effect to attract water from the atmosphere, as well as from the dermis toward the stratum corneum (outer layer of epidermis). Examples of humectants include glycerol, sorbitol, glycerin, urea, lactic acid, and hyaluronic acid (this is present naturally in skin). Since these products pull water from underlying tissue layers, they can actually have a drying effect at times. They also have the propensity to become irritants if used excessively. Like barriers/occlusives, humectants are somewhat bothersome to use due to the ‘tacky’ feeling left on the skin. This is one reason why alcohol in various formulations is added to moisturizers, as it mitigates the ‘tacky’ effect by allowing some of the moisture on the surface of the epidermis to evaporate. Humectants are best utilized immediately after showering or bathing to trap moisture into the skin. These products aid in the treatment of desiccated skin in individuals with multifactorial skin issues such as those that occur with lymphedema and eczema.
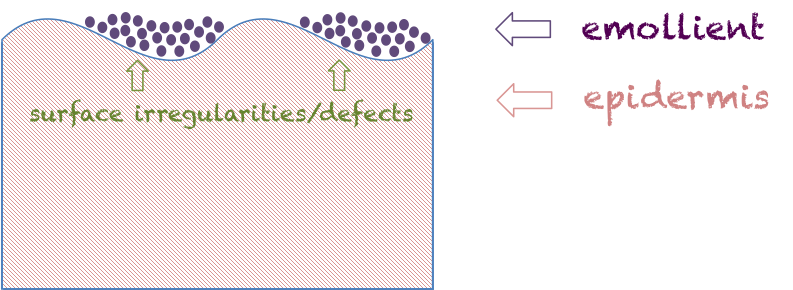
Emollients
Emollients are typically lipids (fats and oils) that can improve the appearance of the skin by filling in defects between skin cells, and make the skin more soft and flexible. Examples include lanolin, paraffin, ceramides, and silicones. Many emollients are also humectants, and both can fill irregularities in skin texture to rapidly improve the texture and appearance of skin. Some emollients such as mineral oil or castor oil can also function as barriers/occlusive. It should be noted that while many humectants have emollient properties, not all emollients are considered humectants. Emollients can be especially useful for individuals who suffer from corticosteroid-induced dermal atrophy or other conditions that impact the texture of the skin.
After reviewing the terms, it becomes apparent that some agents possess an amalgam of properties from more than one of the above categories, and products often contain combinations of these to provide a synergistic effect or to diminish the less desirable qualities of certain skin care products. This is often essential for treatment of complex integumentary issues, even on the same patient at different stages of healing/treatment. I hope this overview leaves you feeling more prepared to analyze the sometimes overwhelming ingredient lists and choose the best skin care product for your patient!
Sources:
ZD Draelos. New Treatments for Repairing Impaired Epidermal Barrier: Skin Barrier Repair Creams. Clinics in Dermatology 2012;30(3):345-8.
Image Source:
Samantha Kuplicki. Used with permission.
About the Author
Samantha Kuplicki is board certified in wound care by both the American Board of Wound Management as a Certified Wound Specialist (CWS) and by the Wound, Ostomy and Continence Certification Board as a Certified Wound Care Nurse (CWCN) and Certified Foot Care Nurse (CFCN). She serves on the American Board of Wound Management (ABWM) Examination Committee and also volunteers for the Association for the Advancement of Wound Care.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.