Preventing and Treating Skin Tears in Older Adults: What You Need to Know
January 27, 2021
Editor's Note: This blog was originally published in June of 2017. It was revised and republished in January of 2021.
Most of us are familiar with the terms "prednisone skin," "thin skin," "fragile skin," or "easily bruises." One or all of these phrases are commonly used to describe our geriatric population's aging skin. As we age, so does our skin. Older adults have older skin. Skin loses elasticity and often gains wrinkles. Skin conditions that may never have been present earlier in life can crop up with aging. Keep in mind that the environment and different exposures (to sunlight, smoking, and stress) can cause our skin to age differently. Additionally, certain drugs, obesity, diet or lifestyle, habits, exercise, repetitive movements, and family history can also influence how our skin ages. Exposure to radiation (for cancer treatment) can also cause skin changes several years after treatment is complete. Regardless of the reason, as we age, our skin composition changes, and undoubtedly the risk for skin tears increases.
How Skin Tears Occur
You may notice that your older adult patient bruises just by bumping into the bed rail or that the tape used to secure gauze after a blood draw seems to tear their skin; these problems are not uncommon. Although prevalent, skin tears are usually easily treatable and, in some cases, preventable.
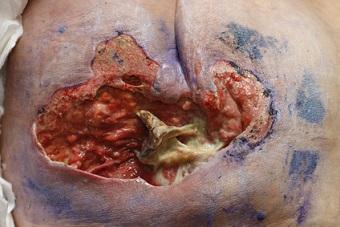
Skin tears usually occur as the result of an accident (bumping into something, such as a doorknob, wheelchair pedal or leg, or other object). Sometimes skin tears can result from direct trauma, such as removing tape or dressing. Direct trauma is sometimes also referred to as the “trigger injury” that initiates a skin tear, which can evolve into another type of wound (venous wounds on the legs, more commonly). Prevention is always best, just as with pressure injuries. However, if we're unable to prevent, then we must treat and heal. Usually, when left undisturbed and protected with a dressing, skin tears resolve quickly, but they can be recurrent.
Treatment and Prevention Strategies for Skin Tears
When a skin tear is first noticed, it is important to attempt to replace the "skin flap" or piece of skin that was torn. With a large skin tear, sometimes wound closure strips can be helpful, but with small skin tears, they're often not needed. A non-adherent wound contact layer, along with bordered foam dressing, usually does the trick to cover. Dressing changes depend on the amount of drainage; some wound dressings can be left in place for a week, whereas others are changed on Monday, Wednesday, and Friday or biweekly. It is helpful to mark the direction with arrows on the secondary dressing, so that when it is removed, the skin flap is left in place and is not torn in the opposite direction.
Alginates or more absorptive dressings are also handy if there is a lot of drainage, a weepy leg, and so forth. Moreover, dressings impregnated with silver can be used as needed for infection. The antimicrobial properties of silver, just like antibiotics, should not be overused. When using silver or other antimicrobial dressings, it is important to re-evaluate wounds frequently to determine continued need.
In terms of prevention, protective arm sleeves are helpful. The use of paper tape or gentle-release tape is also a better alternative to nylon tape, when it comes to sensitive or aging skin. In addition, it is important to moisturize dry skin routinely with an appropriate moisturize barrier. As we age, hydrating dry skin helps to replenish missing skin and keep skin healthy and intact. Oral hydration is important as well. I am sure we've all heard the saying, "a dry cell is a dead cell!"
For bedside nurses in an inpatient setting, having a protocol for skin tears, pressure injury prevention, incontinence management, or other skin issues is often helpful. A skin tear protocol will help to increase rates of healing, ensure that evidence-based treatment is applied initially, and decrease pain during dressing removal.
About the Author
Holly is a board-certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.