Prevention: Hospital-Acquired Conditions in Your Facility
January 31, 2022
Introduction
Hospital-acquired conditions (HACs) arise while a patient is in the hospital being treated for an initial, separate illness or injury. Patients are further harmed as a result of these conditions. Approximately 5% to 10% of hospitalized patients in the United States are afflicted with HACs each year, and the health care system is burdened by $20 billion yearly.1 Medical errors that fall into one of the established categories of HACs are tracked nationally. To calculate the HAC score, the total number of reported errors is taken into account. Certain HACs that occur frequently, can cause significant harm, and are generally preventable based on available research are the conditions that hospitals and health care practitioners concentrate on minimizing.2 Among the top conditions are pressure injuries. Pressure injuries affect more than 2.5 million people in the United States each year, according to the National Institutes of Health. These skin lesions cause discomfort, as well as an increased risk of serious infection and increased use of health care resources.2
Common Hospital-Acquired Conditions
The Agency for Healthcare Research and Quality has developed a toolkit to help reduce the HACs listed here. Through an interdisciplinary approach to patient care, the goal of this toolkit is to assist hospital personnel in the implementation of effective processes.3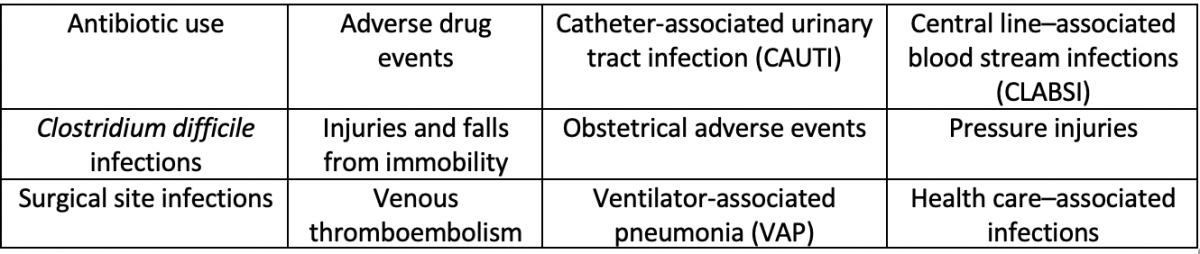
Steps to Prevent Hospital-Acquired Conditions
To provide quality improvement and prevention of pressure injuries and other HACs, a process should be implemented to help facilities prevent avoidable conditions and infections. Studies have shown that formal education and training for health care professionals enhance compliance with best practices, including hand hygiene, infection control, safety culture, and antibiotic stewardship in prevention of health care-associated infections (HAIs).4
Hand Hygiene
Proper hand hygiene is the most important, simplest, and least expensive means of reducing the prevalence of HAIs, as well as the spread of antimicrobial resistance (AMR). By cleaning hands, health care workers can prevent the spread of microorganisms, including those that are resistant to antibiotics and are becoming difficult, if not impossible, to treat. The 5 moments for World Health Organization (WHO) hand hygiene are essential in performing effective hand hygiene.5
- Before touching a patient
- Before clean or aseptic procedures
- After bodily fluid exposure risk
- After touching a patient
- After touching patient surroundings
Environmental Hygiene
Environmental hygiene is a basic principle of infection prevention in medicine. The surfaces in a contaminated hospital play an important role in infection by Clostridium difficile and multidrug-resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE). Therefore, proper hygiene of surfaces and equipment that is in contact with patients and medical professionals is necessary to reduce exposure. Evidence supports the hypothesis that hospitals can function as notable reservoirs for many in-hospital pathogens in a variety of environments, including surfaces, medical devices, and water systems.5
Screening Patients
Isolating patients with high levels of resistant microbial strains prevents patient-to-patient transmission. Quarantine measures need to be integral parts of infection prevention and control programs, but they are often inconsistent. Quarantine measures are expensive, time consuming, and often unpleasant for patients. Their objective is to engage in clinical contact, which may result in the transmission of a pathogen from an infected or colonized patient to another patient, a hospital visitor, and then another patient, or the infection or colonization of the microorganism itself.5
Surveillance
Surveillance systems are widely recognized for their ability to assess local exposure to HAI and AMR. This assessment ability aids in early detection of HAI, including identification of clusters and outbreaks. HAI surveillance systems are integral parts of both national and corporate infection prevention and control programs. The national surveillance system also must be an integral part of the public health system. However, recent data from an AMR global situational analysis showed that many regions reported monitoring obstacles, such as inadequate laboratory capacity, infrastructure, and data management.5
Antibiotic Stewardship
Optimal infection control programs have been identified as important components of a comprehensive AMR management strategy, primarily by limiting the transmission of resistant strains between patients. However, proper use of antibiotics is also required for successful AMR containment in acute care facilities. An antibiotic stewardship program (ASP) helps reduce exposure to antibiotics, decrease Clostridium difficile infection rates, and minimize medical costs. Most antibiotic management activities affect multiple organisms at the same time, with the primary purpose of preventing the development of antibiotic resistance. Therefore, an ASP can be seen primarily in the context of horizontal transmission prevention.5
Following Guidelines To prevent infection successfully, it is essential to have up-to-date insights into the mechanisms of microbial spread, as well as strategies to prevent infection. Although many infection control measures focus on reducing microbial infections, it is just as important to identify measures to reduce the severity of infection. Both the WHO and the US Centers for Disease Control and Prevention (CDC) have recently published guidelines for the prevention of surgical site infections (SSIs). Knowledge and awareness of infection prevention and control measures are often inadequate, and there is a large gap between the best evidence of SSI prevention and clinical practice.5
Safety Culture
Patient safety means to ensure the elimination of risk of avoidable harm to the patient during the medical process, thereby decreasing the possibility of unnecessary medical-related harm to an acceptable minimum. Improving patient safety in today's hospitals around the world requires a systematic approach to addressing HAIs and AMR. The two go hand in hand. Conditions and infections develop during the course of treatment and extend hospital stays. These extended stays can result in serious illness and death in the patient (morbidity and mortality). HAI is considered a detrimental outcome and is often preventable, so it is considered an indicator of poor patient care quality, adverse events, and patient safety issues.5
Automated Clinical Workflow
Integrating an automated clinical workflow can help prevent HACs by systematically assessing barriers and using evidence-based practices. Clinical workflow is aimed at improving the functionality of the health care system, with the ultimate goals of streamlining the process and providing patients with the best health experience possible. Clinical workflow can be improved so that clinicians can perform jobs in less time or with less effort, reduce the time spent waiting for others to complete tasks, communicate and collaborate more efficiently, and provide better care to patients.6
Conclusion
Patients who are in the hospital for treatment of a different illness are at risk of developing harmful HACs. Hospitals and health care providers are working toward minimizing specific HACs that occur frequently, cause significant harm, and are generally preventable based on available research. Implementing a systematic process while prioritizing education will help optimize overall outcomes.
References
- Centers for Disease Control and Prevention (CDC). CDC at work: preventing healthcare-associated infections. Accessed December 17, 2021. https://www.cdc.gov/washington/~cdcatWork/pdf/infections.pdf
- Agency for Healthcare Research and Quality. AHRQ tools to reduce hospital-acquired conditions. Last reviewed June 2021. Accessed December 16, 2021. https://www.ahrq.gov/hai/hac/tools.html Agency for Healthcare Research and Quality. Preventing pressure ulcers in hospitals. Last reviewed October 2014. Accessed January 5, 2022. https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressure…
- Agency for Healthcare Research and Quality. AHRQ’s healthcare-associated infections program: tools & resources to prevent HAIs. Accessed January 5, 2022. http://www.ahrq.gov/professionals/quality-patient-safety/hais/index.html
- Global Alliance for Infections in Surgery. 7 strategies to prevent healthcare-associated infections. Accessed December 17, 2021. https://infectionsinsurgery.org/7-strategies-to-prevent-healthcare-asso…
- Improving clinical workflow. HIPAA Journal. n.d. Accessed December 17, 2021. https://www.hipaajournal.com/improving-clinical-workflow/
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.