Traumatic, Full-Thickness Wounds: How an Advanced Dressing Can Help
November 9, 2023
Introduction
A recent case presented in a poster at SAWC emphasizes the unique nature of traumatic, full-thickness wounds. Full-thickness wounds due to trauma, especially those left out to the open for extended periods, are not only at risk of becoming infected and chronic but can also greatly negatively impact patient quality of life. A study from 2021 on the correlation between trauma wound severity and infection rates found an infection prevalence of 6% of the 150,948 patients in the study.1 Of those with infection, approximately 10% had a greater mortality rate in the hospital than those without infection.1
Delayed or lack of access to care can increase risk of complication for these patients, and although it is reported that “the majority of the United States has access to trauma care within an hour,” there are approximately 30 million US residents who face barriers such as insurance status, income level, and location.2 For these reasons, wound care professionals should ensure the use of standard of care and best evidence based practices when managing these wounds.2
In addition to standard of care like sharp debridement, bioresorbable polymeric matrixes with antimicrobial properties can prove invaluable in the treatment of these wounds. A 2020 study found that the use of a bioresorbable polymeric matrix impregnated with silver was effective at moving stalled, chronic wounds out of the inflammatory phase and into the proliferative phase.3 In tandem with its antimicrobial properties, as a result of slow-release ionic and metallic silver present in its layers, these matrixes support the migration of keratinocytes and other cells across the wound bed by acting as a scaffold. Bioresorbable polymeric matrixes impregnated with silver can aid in treating complicated wounds with risk of infection.3
Case Study
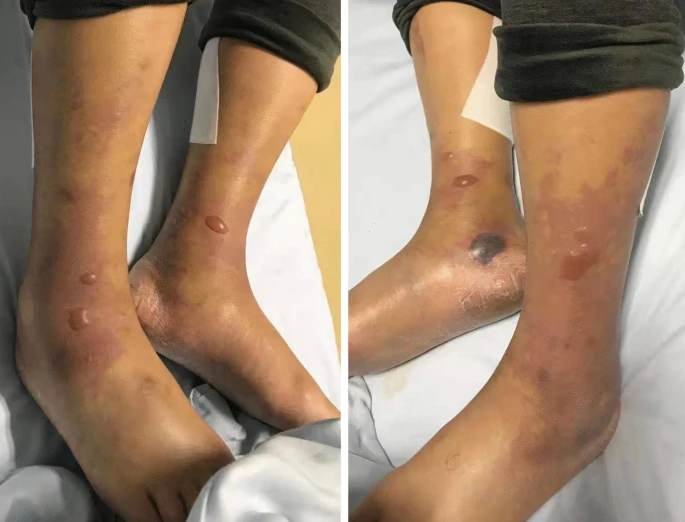
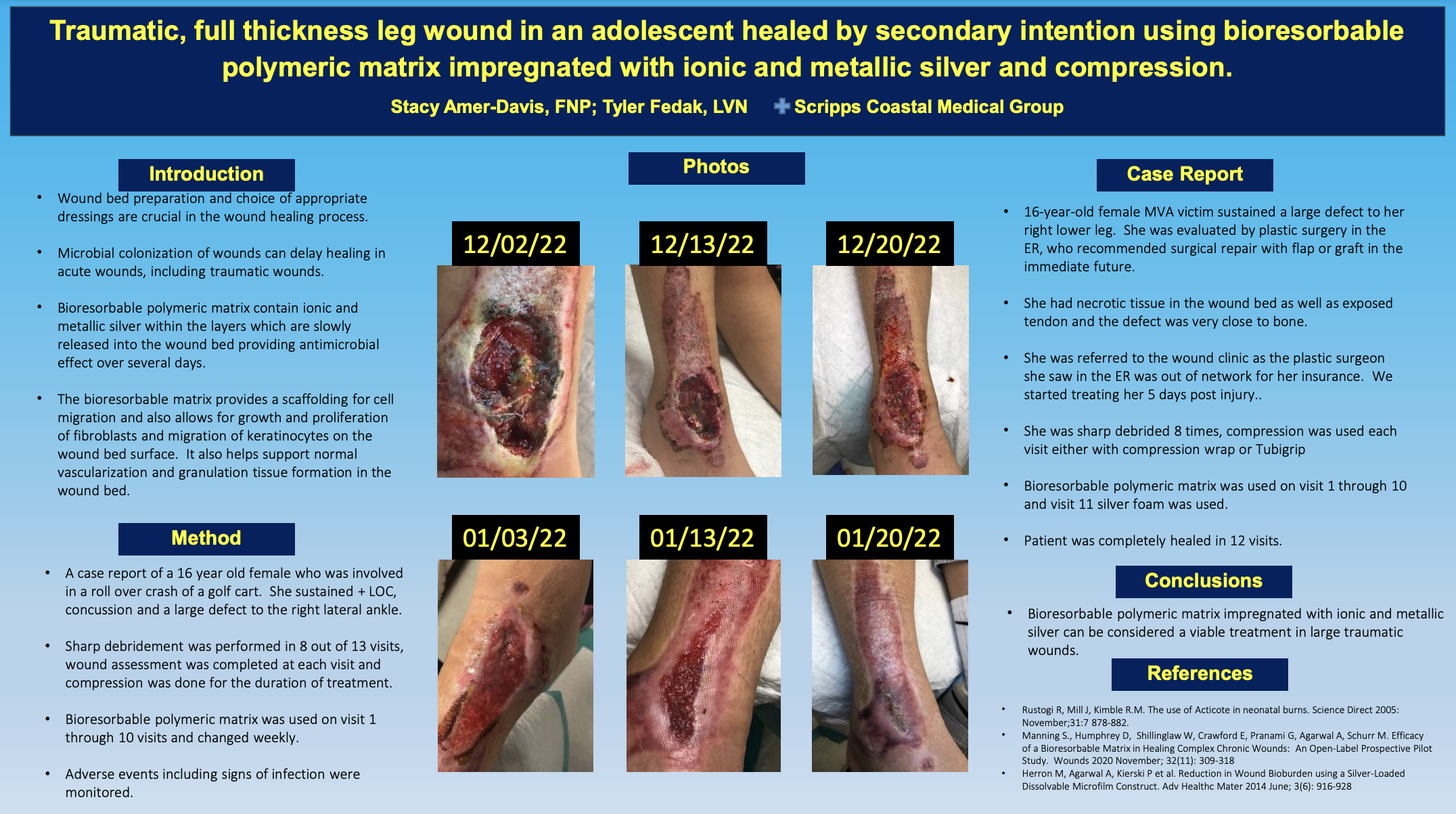
In their poster featured at SAWC Fall 2023, Stacy Amer-Davis, FNP and Tyler Fedak, LVN presented a case study where they showed the efficacy of a bioresorbable polymeric matrix impregnated with ionic and metallic silver.4 A patient with a full-thickness traumatic wound of the lower leg checked into their facility after their insurance did not cover the recommended surgical flap or graft initially suggested by the ER. Due to the 5-day delay in care and necrotic tissue in the wound bed, infection was suspected. Tendon and bone were visible.4
The providers used a polymeric matrix impregnated with silver as the primary dressing following each sharp debridement. Compression and a controlled ankle motion (CAM) boot were also used at each visit. After 12 visits to their facility, the wound was completely healed. Subsequently, the poster presenters posited that use of a “bioresorbable polymeric matrix impregnated with ionic and metallic silver can be considered a viable treatment in large traumatic wounds.”4
Conclusion
With barriers like suspected infection, the providers were tasked to heal a full-thickness wound by secondary intention and achieved wound closure.4 For complicated wounds like traumatic, full thickness wounds with suspected infection, the proper use of dressings can have a larger impact than one may assume. Utilizing dressings effectively is reported to decrease healing time, lower care costs, and increase patient quality of life.5 Wound care professionals should use advanced dressings that not only provide a moist wound environment but provide properties like antimicrobial resistance as well.
References
- Komori A, Iriyama H, Kainoh T, et al. The impact of infection complications after trauma differs according to trauma severity. Sci Rep. 2021;(11):13803. https://doi.org/10.1038/s41598-021-93314-5
- Carr B, Bowman A, Wolff C, et al. Disparities in access to trauma care in the United States: a population-based analysis. Injury. 2017; 48(2): 332-338. doi: 10.1016/j.injury.2017.01.008
- Manning SW, Humphrey DA, Shillinglaw WR. Efficacy of a bioresorbable matrix in healing complex chronic wounds: An open-label prospective pilot study. Wounds. 2020;32(11):309-318. https://www.hmpgloballearningnetwork.com/site/wounds/article/efficacy-b…
- Amer-Davis S, Fedak T. Traumatic, full thickness wound in an adolescent by secondary intention using bioresorbable polymeric matrix impregnated with ionic and metallic silver and compression. Poster presented at: SAWC Fall 2023; November 2-5: Las Vegas, NV.
- ritto EJ, Nezwek TA, Popowicz P, et al. Wound Dressings. In: StatPearls [Internet]. StatPearls Publishing; 2023: https://www.ncbi.nlm.nih.gov/books/NBK470199/
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.