Venous vs. Arterial Wounds: Differential Diagnosis and Interventions
September 1, 2020
Lower extremity ulcers, such as venous and arterial ulcers, can be complex and costly and can cause social distress. An estimated 1% of the adult population is affected by vascular wound types, and 3.6% of those affected are older than 65 years of age. Many factors contribute to lower extremity wound chronicity, including venous disease, arterial disease, neuropathy, and less common causes of metabolic disorders, hematological disorders, and infective diseases.1 A total of 15% to 20% of lower limb ulcers have a mixed etiology.
Venous Ulcers
The venous system normally decreases in pressure during exercise or when the calf muscle pump is in use. When muscles are relaxed, the valves in the perforating veins should prevent reflux and maintain a low pressure in the deep venous circulation. If there is damage to the veins, pressure remains high, and therefore valves are deemed incompetent. Sustained venous hypertension leads to venous leg ulcers caused by chronic venous insufficiency.1
Arterial Ulcers
Arterial ulcers are caused by reduced arterial blood supply to the lower limbs secondary to atherosclerotic disease of the larger arteries. When there is concurrent hypertension in the intimal layer of an artery, further damage will occur. Results of poor circulation or decreased arterial blood supply are tissue hypoxia and tissue damage.1
The Importance of Vascular Assessment
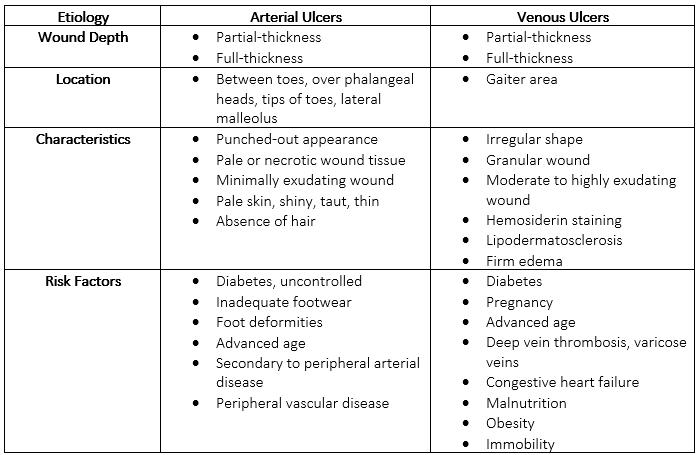
Performing a thorough systematic assessment of the patient is vital for correctly diagnosing underlying causes and optimal treatment in these patients. Differentiating venous from arterial wounds should be performed by including an evaluation of anatomical location, wound shape, and wound color as a baseline, followed by vascular studies as indicated. Inappropriate treatment can lead to wound deterioration and possible limb loss or death. Utilizing various strategies and newer modalities in patients with lower extremity wounds can lead to not only better healing outcomes, but also better quality of life and lower financial burden on the patient.2
Accurate vascular assessment is necessary to determine correct diagnosis and treatment. Providers should examine and document both legs, including palpating pulses, edema if present (pitting or non-pitting), skin pigmentation changes, varicose veins, eczema, atrophie blanche, and lipodermatosclerosis. Determine sensation, activity level, and range of motion. A thorough wound assessment should include evaluation of wound site, size, depth, tissue type(s), exudate, edges or margins, periwound, and surrounding skin.
Vascular Studies
It has been estimated that as many as 50% of lower extremity amputations in the United States have been performed without prior vascular testing.3 This is primarily because providers have made the diagnosis based on ulcer anatomical location, characteristics, and morphology. However, validation of vascular disease requires laboratory studies, diagnostic testing, and a comprehensive functional assessment as indicated. Venous duplex testing is most commonly used to diagnose venous disease.4 Venography is known as the "gold standard" for diagnosis, but because of cost and associated morbidity, as well as availability of non-invasive tests, it is not often ordered or performed. Providers should consider various factors when selecting non-invasive imaging to minimize risk in patients, including history of ulcerations, duration, and recurrence.
In patients whose pulses are difficult to palpate, Doppler ultrasound imaging can be used. The ankle-brachial index (ABI) measures peripheral tissue perfusion, with an ABI lower than 0.8 indicating arterial disease. Therefore, the lower the ABI result, the more likely it is that the patient is at risk for a revascularization procedure or amputation.5
Edema Management
When the capillary filtration system of the lower extremities is overwhelmed by lymphatic drainage, edema develops, caused by an accumulation of fluid in the interstitial space. Chronic edema in one or more lower extremities often indicates venous insufficiency. The simultaneous presence of hemosiderin deposition and edema warrants a diagnosis of chronic venous insufficiency. The "gold standard" therapy for venous ulcers is compression therapy. Compression therapy may be contraindicated for patients with a mixed etiology of arterial and venous insufficiency. The goals of treatment are to manage edema, improve venous reflux, and move wounds toward a healing trajectory.
Bandages used for compression therapy can range from one layer to various layers to achieve the prescribed mm Hg of gradient pressure. Compression stockings should be used in patients after deep vein thrombosis to prevent post-thrombotic syndrome. Pneumatic compression pumps deliver variances of pressure gradient, inflation, and deflation cycles. Leg elevation should be above heart level to help reduce venous pressure.
Interventions
Wound cleansing and debridement are at the core of expediting healing rates. Using one or more of the five methods of debridement will help move wounds toward healing. Patients treated with sharp debridement have shown significant reductions in wound size compared with those patients not treated with debridement. Good skin care is essential in prevention of skin breakdown and development of venous ulcers because of the high incidence eczematous stasis dermatitis. Emollients and topical steroidal agents are effective in treating this skin condition.
Dressing options include hydroactive, hydrocolloid, films, absorbent dressings such as alginate, foams, and super absorbent dressings. These dressings help maintain moist wound healing, provide thermoregulation, and enhance wound healing. Collagen dressings with or without silver are used to decrease matrix metalloproteinases and manage bacterial levels. Antimicrobials and antiseptics are used to improve healing by eradicating biofilm and managing free radicals.
Cadexomer iodine, povidone, iodine, medical-grade honey, silver, sodium hypochlorite, peroxide-based preparation, and hypochlorous acid have been shown to support wound healing progress. Surfactants and wound cleansers help remove exudates and contaminants in the wound bed. Advanced wound care therapies include cellular and/or tissue-based products and skin grafting used as a secondary therapy when standard of care fails. Medications can also be considered in patients with lower limb ulcerations. Medications include pentoxifylline, aspirin, statins, phlebotomics, and antibiotics if infection is suspected.
Conclusion
Most lower extremity chronic ulcers are caused by vascular conditions. A comprehensive history and physical assessment are essential in early identification, diagnosis of correct etiology, and development of the most effective care planning. Including patients in their care and education is key in optimizing wound management and minimizing recurrence of ulcerations.
References:
1. Grey JE, Harding KG, Enoch S. Venous and arterial leg ulcers. BMJ. 2006;332(7537):347–350. doi: 10.1136/bmj.332.7537.347
2. Kahle B, Hermanns HJ, Gallenkemper G. Evidence-based treatment of chronic leg ulcers. Dtsch Arztebl Int. 2011;108(14):231-237.
3. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-141.
4. Min RJ, Khilnani NM, Golia P. Duplex ultrasound evaluation of lower extremity venous insufficiency. J Vasc Interv Radiol. 2003;14(10):1233-1241.
5. Meyers B. Wound Management. 2nd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2008:234.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











