Wound Documentation: Commonly Confused Wound Care Terms
October 17, 2019
Documentation is a huge part of our practice as wound care nurses. It is how we take credit for the care we provide to our patients and how we explain things so that other providers can understand what is going on with the patient, and it is used for legal and billing purposes as well. Wound care is a specialized practice that involves specific documentation. There are times when this specific documentation can be confusing or unclear. As with any area of nursing, it is important to document the facts and to keep in mind the purposes of documentation, which are to paint a picture of the care provided to the patient in a timely manner with concise information and to facilitate care coordination among the members of the health care team. In wound care, certain concepts are at times documented more incorrectly or incompletely than other concepts. Here we explore a few of these concepts.
Potential Documentation Errors
Partial- vs. Full-Thickness: The Presence of Granulation Tissue
Granulation tissue is present in full-thickness wounds. You would not see granulation tissue in a stage 2 pressure injury—you could see pink or red non-granular tissue, a shallow wound bed, partial-thickness tissue loss, or epidermis.
Slough vs. Purulence
Slough is stringy, moist, and yellow, and as it is debrided, it can liquefy or dissolve. Purulence is the presence of pus, and it usually is associated with erythema, odor, redness that does not improve with elevation of a limb, pain, increase in drainage, fever, chills, nausea, or vomiting.
Moisture-Associated Skin Damage vs. Pressure
Moisture-associated skin damage (MASD) is irregularly shaped, not round or punched out, and usually is not isolated over a bony prominence. MASD is usually superficial (partial-thickness) and is present in patients who are incontinent, diaphoretic, or frequently moist as a result of a leaking drain, tube or wound. MASD certainly has the potential to evolve into a pressure injury. However, our goal is to catch it early, identify and correct the cause, and topically treat the skin damage.
Dependent Rubor vs. Erythema
Dependent rubor is when the limb is red when in a dependent position. Normal coloring returns when the limb is elevated. Erythema is the presence of redness in any limb position.
A Closer Look at Wound Characteristics
Let's break down some of these concepts…
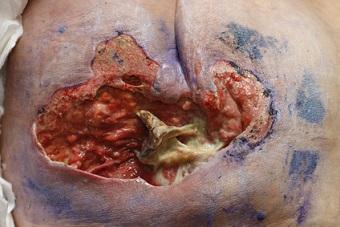
Partial- vs. Full-Thickness
Partial-thickness wounds consist of damage to the first two layers of the skin: the epidermis and the dermis. These wounds are superficial. They manifest with a pink-red wound base without slough. Partial-thickness wounds do not have granulation tissue because they heal by epithelialization and regeneration of the epidermis across the wound bed. Some examples of common partial-thickness wounds are abrasions, skin tears, medical adhesive-related skin injuries (MARSI), MASD, and stage 2 pressure injuries. Full-thickness wounds extend beyond the first two layers of the skin damaged by partial-thickness wounds (the epidermis and the dermis). These wounds penetrate subcutaneous tissue and may involve bone, muscle, or tendon. Necrotic tissue such as eschar or slough may also be present in these wounds. Full-thickness wounds contain granulation tissue and heal by granulating inward from the bottom up, contraction, and finally epithelialization. A deeper wound requires a more in-depth healing process. Sometimes unstageable pressure injuries or deep tissue injuries present a challenge when determining partial- vs. full-thickness. These two wound stages typically evolve to full-thickness tissue damage. When determining the level of tissue damage within a wound, it is always important to look at the depth of tissue involved (epidermis, dermis, or extending beyond the dermis). If you're not sure, simply describe what you see, and consult with your wound care specialist.
Slough vs. Purulence
It is important to look at the entire picture here. The periwound skin can provide some important information here as well—is there erythema, fluctuance, any other sign of infection? Or, is there more stringy, yellow, liquefying slough related to the debriding agent being used? Is there an odor? Remember always to use your senses when completing a thorough wound assessment. More information on this topic is available in an earlier blog: Assessing Wound Tissue and Drainage Types: Slough Versus Purulence.
Dependent Rubor vs. Erythema
This is an important concept to understand to best treat the cause of the skin condition. Dependent rubor and erythema have different causes and therefore should be managed differently. Dependent rubor, as the name suggests, is seen when the legs are in a dependent position. The legs appear red but return to a normal color when they are elevated. True erythema typically does not resolve when the legs are elevated. Additionally, some indicators of a vascular process could be hemosiderin staining and changes consistent with venous stasis or venous dermatitis. Understanding the differences between cellulitis and vascular issues is important when formulating a treatment plan for leg ulcers. It is always best to take an interprofessional approach and formulate an interdisciplinary plan of care. Again, if you're not sure, just describe what you see in your charting, and consult with your wound care specialist.
Take-Away Points on Wound Documentation
- Understanding the etiology of a wound is essential before developing a treatment plan.
- Documentation should be clear, concise, and factual, and it should paint a picture of the care provided.
- If you're not sure of what you’re looking at, just describe what you see (vs. identifying etiology or cause) and consult with your wound care specialist.
"The only stupid question is the question that is never asked." ― Ramon Bautista
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.